Myth: Surgery is the end of the Endometriosis care journey
Fact: Endometriosis care requires constant life-style changes and medical support
As is the case with many other chronic illnesses, Endometriosis requires major life-style changes which continue beyond the point of surgery. Although surgery greatly improves the quality of life for most patients such as myself, it is not the end point. Something that I found difficult post-surgery was people asking “so are you better now?” Yes to a degree, but living with a chronic illness is not a linear journey. It is more like a rollercoaster – some stretches are smooth and pleasant, others are the horrific upside-down-stomach in the mouth kind of feeling you get when they veer in various directions.
Living with Endometriosis – and any other chronic illness – requires constant life-style maintenance. Changes I have made include a complete overhaul of my diet, a reduction in alcohol and caffeine consumption, giving up sports I love for low impact physical exercise, as well as altering both my job and social life activities. Alongside this, it means being in constant discussion with medical professionals.
I am currently four months post-surgery and still I keep a daily symptom diary. Recording symptoms is absolutely vital, especially for approaching the more problematic and dismissive GPs. I now religiously record any medications I start, what day I began them, what time of day I take them. I record the days I exhibit extreme nausea and through this I have been able to figure out the ‘trigger foods’ and make subsequent further changes to my diet. I keep track of pain levels and do my best to correlate them to physical activities, in order to avoid overdoing things. I also record any blood tests, medical appointments, phone call discussions and most recently a visit from the paramedics.
Keeping track of what goes wrong takes so much time; inadvertently I have become the administrator of my illness and I know this is the case for many chronic illness patients. The time spent on hold, the numerous phone calls, booking of appointments, re-booking due to Covid-19 disruption, travel to and from hospitals; all of these alongside the usual daily routine of work, social life and domestic maintenance.
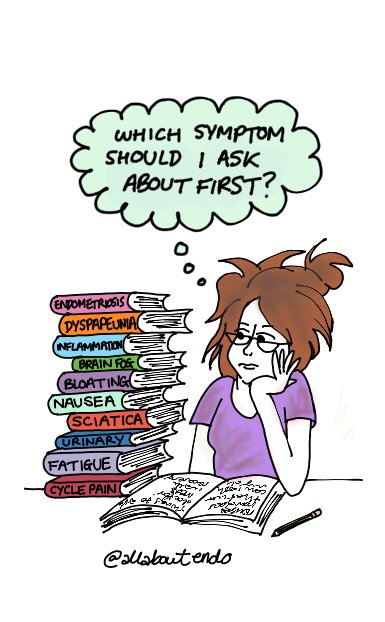
Given the array of symptoms I experience and the fact that GP appointments are a maximum of 10 minutes, I often end up having to prioritise the symptoms that get discussed, leaving others to go untreated for another week, two weeks and before you know it, months. This is very much the case when I visit new GP surgeries, or different hospitals, as not all medical systems have their databases shared and streamlined. As a result, you often end up explaining everything repeatedly, which is why it’s so vital to have a reliable GP and consultant who you can return to. This however, is very rarely the case and more often than not I have been treated by an array of different medical professionals, some of whom have been a lot more sympathetic than others. I had one GP who dismissed my suggestion of dietician advice retort that there was no correlation between Endometriosis and gluten allergies. I had another tell me I was “too young” to have sciatica. I even had one tell me I didn’t have Endometriosis – without even referring me for a diagnostic laparoscopy. The list of disappointing appointments is endless and is a core reason why I started this blog and comic strip. Knowing what I have learnt in the past few years would have made all the difference when I was first diagnosed.
For patients that don’t have a symptom diary, I cannot recommend this enough. I’ve had some very difficult GPs in the past and the symptom diary has been a life saver in the moments where I felt on the brink of tears with exasperation. Endometriosis UK have a Pain and Symptom Diary available on their website and it is a brilliant method to allowing you to more fully understand your symptoms, especially in the challenging moments when doctors refuse to acknowledge them.
***
On a non-Endometriosis related note, I recently bought a digital tablet so that I can begin experimenting with digital drawing! It’s a very different way of working, but I am enjoying the change and experimentation that comes with adapting my drawing style and it’s great to be able to draw in bed more easily on flare up days!
[Image description: Camilla sits at a desk with her head resting on her hand, glasses on and hair tied up in a messy bun. She has paper notes in front of her alongside a pencil and has a disgruntled expression on her face. Beside her is a pile of different coloured books, with titles from top to bottom: Endometriosis, Dyspareunia, Inflammation, Brain Fog, Bloating, Nausea, Sciatica, Urinary, Fatigue, Cycle Pain. A mint coloured through bubble above her head reads ‘which symptom should I ask about first?’]