Myth: Hormonal treatments are a cure for Endometriosis
Fact: Endometriosis can not be cured, but symptoms can be managed through various hormonal treatments
There are a lot of misconceptions that surround Endometriosis; a core one being that hormonal treatments provide the ultimate solution. This is not the case as the only current way to effectively treat Endometriosis is through excision surgery (more on this in later posts). Yet hormones are in many cases very helpful in managing and suppressing symptoms.
As Endometriosis responds and grows when exposed to the female hormone oestrogen, hormonal treatments are often employed to block or reduce the production of oestrogen in the body [1]. Oestrogen production is the reason why Endometriosis symptoms are heightened during menstruation, as during each cycle there is a rise and fluctuation in hormones.
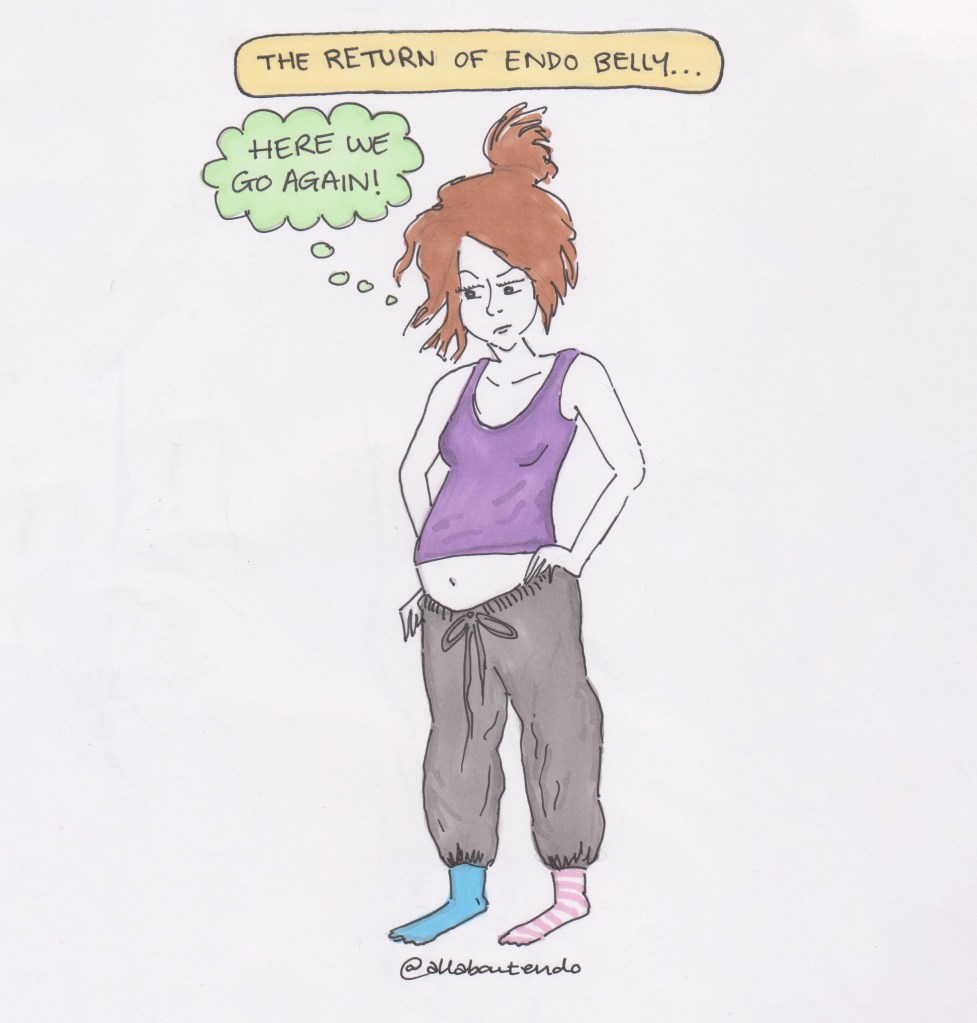
This results in bloating, often referred to as ‘endo belly’; the severity of which varies from patient to patient. The bloating is uncomfortable, painful and in my experience always occurs at the least convenient moment (ie. just when I’ve decided on an outfit I was planning to wear which is no longer comfortable with the onset of ‘end belly’)!
91.25% of Endometriosis patients indicate bloating as a symptom [2]. Bloating is not limited to periods of menstruation, and can occur in any individual with Endometriosis at any time [3]. ‘Trigger foods’ such as spice, alcohol, caffeine, gluten and dairy can exacerbate this – so many patients cut these to help manage symptoms. I found overhauling my diet greatly reduced my pain and inflammatory symptoms and was a life saver whilst I waited for surgery – although I will admit reducing my caffeine intake to one coffee a day has been a challenge! Again however, diet changes are merely a means of managing rather than treating symptoms and should be accompanied by other things such as hormonal treatments.
The use of hormonal blockers prevents the Endometriosis from growing and helps relieve symptoms such as bloating. Note however that this provides purely temporary relief – as soon as patients stop taking the hormones, the Endometriosis will continue to grow. This is because the hormones put Endometriosis patients in a temporary state of pregnancy, or a temporary state of menopause [4].
I remember after one bad flare up last year, which resulted in two urgent trips to the doctor followed by an emergency hospital visit; being offered the menopause as interim treatment while I waited for my surgery. I felt like a massive hole had opened in the floor and would swallow both me and my hospital chair up any minute given my shock at this suggestion. Never before had this been suggested as a form of treatment, so I knew nothing about the side effects of medically inducing menopause mid-twenties and was very uncertain about selecting this treatment route.
Any hormonal treatment has side effects, but menopause comes with a whole array including hot flushes, night sweats, skin dryness and insomnia. The risk of medically and prematurely inducing menopause comes with an additional one – the risk of osteoporosis. This condition results in the thinning of bone density which increases the risk of fractures [5]. Needless to say, this was not something I was particularly keen on pursuing. Menopause affects every women somewhat differently and at this point, I was very used to Endometriosis pain being part of my daily life, so was reluctant to throw menopause into the mix even though it would only be a six month treatment. Induced menopause is used only in the short term to reduce the risk of osteoporosis, and is sometimes used in combination with Hormone Replacement Therapy (HRT) to protect bones and blood vessels, thereby reducing the associated menopause symptoms [6].
Needless to say, hormonal treatments all come with various side effects and can be a huge decision in terms of selecting the most suitable route – as each patient will respond differently to things such as the contraceptive pill, Mirena coil, HRT, etc. But this week we have brilliant and exciting news from The University of Edinburgh who have been conducting trials which suggests that Endometriosis could be treated effectively with a cancer drug. Excerpt below:
‘Researchers from the University of Edinburgh found that cells from the pelvic wall of women with endometriosis have different metabolism compared to women without the disease. The cells produced higher amounts of lactate similar to the behavior of cancer cells.
When the cells from women with endometriosis were treated with dichloroacetate, they were found to return to normal metabolic behavior. The scientists also noted a reduction in lactate and an impact on the growth of endometrial cells grown together with the pelvic cells.
Further tests on a mouse model of endometriosis found, after seven days, a marked reduction in lactate concentrations and the size of lesions.’ [7]
This proves that the more resources we put into funding vital research such as this, the more hope we have for improving the lives of the 176 million women worldwide[7] who are living with Endometriosis. It would mean that a straightforward – rather than the usual trial and error – treatment route would finally be available, allowing for longer term improvements to health and reducing the need for multiple surgeries.
[1] EndometriosisUK, Hormonal Treatments for Endometriosis, https://endometriosis-uk.org/hormone-treatments-endometriosis
[2] Moradi, Parker, Sneddon et al., 2019. Maroun et al. (2009)
[3] Centre for Endometriosis Care, EndoBelly: https://centerforendo.com/endobelly
[4] EndometriosisUK, Hormonal Treatments for Endometriosis, Ibid.
[5] Evidently Cochrane, Hormone Therapy for the Menopause after Endometriosis Surgery – Friend or Foe?, Martin Hirsch, March 2015
[6] The University of Edinburgh, Unable to obtain usual treatment or asked to change treatment: https://www.ed.ac.uk/centre-reproductive-health/exppect-endometriosis/covid19-advice-nhs-lothian-endometriosis/covid19-drug-change-advice
[7] The University of Edinburgh, Endometriosis could be treated with new cancer drug, https://www.ed.ac.uk/news/2019/endometriosis-could-be-treated-with-cancer-drug
[Image description: Camilla is stood with her hand on her hips, wearing a purple strappy top and grey tracksuit bottoms. She is wearing mismatched socks and her brown hair is held up in a messy bun. Her facial expression looks cross, as her belly is fully bloated, exhibiting symptoms of ‘endo belly’. A yellow banner above her head reads ‘the return of endo belly’ with a thought bubble reading ‘here we go again’.]